COGNITIVE BEHAVIOURAL THERAPY (CBT)
Cognitive Therapy was developed by Aaron Beck (1979) as a shorter-term therapy with a strong self-help orientation. Cognitive Therapy (considered '2nd wave' CBT) followed on the heels of the pre-existing Behavioural Therapy ('1st wave'), and these were later combined to form the CBT we know today. CBT has a sound evidence-base and enjoys continuous research and development, and it is the therapeutic approach most commonly recommended by the National Institute for Health and Care Excellence (NICE) for a range of psychological problems.
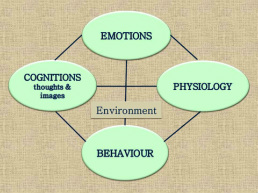
CBT therapists are interested in the interplay between cognitions (e.g. thoughts, images, memories) and emotions (anxiety, low mood, anger etc). We also attend to the behaviours employed as a response to 'negative automatic thoughts', uncomfortable feelings or perhaps physical sensations. For instance, it is natural to want to keep a distance from what we dislike or fear by avoiding certain experiences or places; we may drink too much in order to feel less anxious or sad, withdraw from activities when we feel low, or engage in compulsive behaviours such as checking or washing in an effort to try to calm our worrying thoughts and feelings. When there is a real and present danger, avoidance may be a helpful or even life saving response. But when a feared outcome is in the past, or is unlikely and hypothetical ('what if...?'), we find that those same strategies become restrictive, reducing the quality of our lives and actually adding to our suffering.
CBT therapy is about changing the way we feel by changing the way we think (traditionally, this has included disputing or logically considering the evidence for troubling beliefs) and also by changing the way we behave (road-testing new ways of thinking/acting towards discovering something new about how things actually are and what is possible).
Behavioural changes are usually practiced in small steps, initially as 'experiments' that are reviewed in therapy. Between session tasks (experiments, logs, worksheets etc) extends the therapy process between appointments, which can shorten the overall time in therapy and provide an opportunity to take things forward oneself - and that helps to maintain change when therapy has ended.
ACCEPTANCE AND COMMITMENT THERAPY (ACT)
For over a decade, I have been privileged to offer clients a variant of CBT known as 'ACT' (Acceptance and Commitment Therapy), which has its own ever-growing evidence base. Rather then waging war on our 'distorted' or 'irrational' beliefs (e.g. by challenging/disputing them), ACT teaches ways of responding differently to our own troubling feelings and thoughts (compassionately and from an observing perspective) .
ACT, considered a '3rd wave' CBT approach, was developed by Steven Hayes, Kelly Wilson, and Kirk Strosahl (1989) and is now practiced internationally. It is an empirically-based therapeutic approach that uses mindfulness-based principles (such as acceptance, present moment awareness, observer perspective) alongside the behavioural change methods used in traditional CBT, such as working towards goals using graded (small steps) encounters with previously avoided experience.
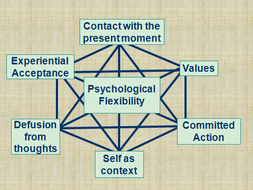
ACT identifies six, inter-related processes that are seen as central to our psychological well-being. Therapy will probably focus on all of these, although with a different emphasis from person to person. The skills you will learn include:
- cognitive 'defusion': learning how to unhook from the content of unhelpful thoughts, images, memories...
- acceptance: learning to be aware of, and open to, our feelings and emotions, with self-compassion
- contacting the present moment: being aware of the here and now, leading to greater self-knowledge and grounding
- developing an 'observing' sense of self - we are more than our thoughts and feelings
- values identification - exploring what is most important to you and using values as a compass to direct decisions and choices
- committed action: following through towards our value-driven goals
See the 'Links' section for ACT resources
